Unmasking the breast cancer crisis in Africa: impact on families and economies

In South Africa, the International Agency for Research on Cancer predicts that breast cancer deaths are predicted to rise by more than a third by 2030.
Image: Unsplash/Angiola Harry
Experts caution that breast cancer is becoming one of Africa's most urgent health and development issues, with disastrous effects on women, their families, and national economies.
Professor Carol-Ann Benn, founder of the Breast Care Centre of Excellence and Chair of the Africa Breast Cancer Council, tells IOL that urgent action is needed to prevent what she describes as a growing catastrophe.
“Breast cancer is now one of Africa’s most urgent health challenges,” Benn told IOL.
Women are being diagnosed at younger ages and often at a later stage, often without access to specialist care, resulting in high mortality rates.
This is not because the disease is more aggressive, but because the healthcare system is slow to reach women with "projections indicating that cases will double throughout the continent by 2045," Professor Carol Benn noted with a great degree of concern.
In South Africa, the International Agency for Research on Cancer predicts that breast cancer deaths are predicted to rise by more than a third by 2030. And when a woman becomes ill in Africa, the impact extends beyond just one person,” Benn added.
She explained that women with breast cancer are often the centre of a family, and key contributors to the economy.
"Women with breast cancer can have adverse effects on their children’s education, household stability, and community wellbeing."
Early Detection and Economic Impact
Benn stressed that early detection is not only a medical imperative, but an economic one.
"Early detection not only saves lives but also economies,” she told IOL.
Treating late-stage breast cancer can be up to twenty times more expensive than early diagnosis. Every year of delayed diagnosis removes women from the workforce, destabilises families, and increases national healthcare costs.
Evidence from Egypt underscores the impact.
For every £1 invested in screening (about R22.50), the country gained approximately £1.38 (around R31) in economic return, saving roughly R562 million in productivity.
Over 60 million women accessed health facilities, more than 33,500 breast cancer cases were detected, and thousands received life-saving treatment free of charge.
"While each country differs, the pattern is clear: early detection is one of the most cost-effective development investments any nation can make,” Benn said.

Professor Carol Benn has paved the way in South Africa for the improvement of women’s health care and the uplifting of women in society, and has opened channels for public awareness of breast health.
Image: Supplied
Premature deaths among women in their prime working years cost billions across the African continent. Globally, such losses amount to US$566 billion in lost productivity."
In South Africa alone, more than US$5 billion - roughly R84 billion - was lost to breast-cancer-related productivity between 2017 and 2023.
“Treating breast cancer effectively enables women to live longer, participate in the workforce, and contribute to their communities,” Benn told IOL.
She further explained that "the single most powerful policy lever is early detection paired with timely, effective treatment. It keeps women healthy, families stable, and economies functioning.”
Early Detection as a national priority
For meaningful change, early-stage diagnosis must become a core pillar of national health strategies across Africa. An exemplary example can be drawn from Egypt’s national programme, which demonstrates that leveraging existing systems - such as community access points, trained personnel, and data infrastructure - produces tangible results.
“Early detection only saves lives when the entire system is built to move women quickly and safely from first concern to care,” Benn explained.
Key priorities include bringing screening to underprivileged communities, an active voice that addresses the social and cultural barriers of not investing in the workforce of breast cancer awareness.
The use of up-to-date, more appropriate technology and building efficient treatment pathways through service delivery and lastly, data-driven decision making to ensure this system responds effectively.
Early detection does not begin in a hospital; it begins in homes, churches, workplaces, and community circles - Professor Carol Benn
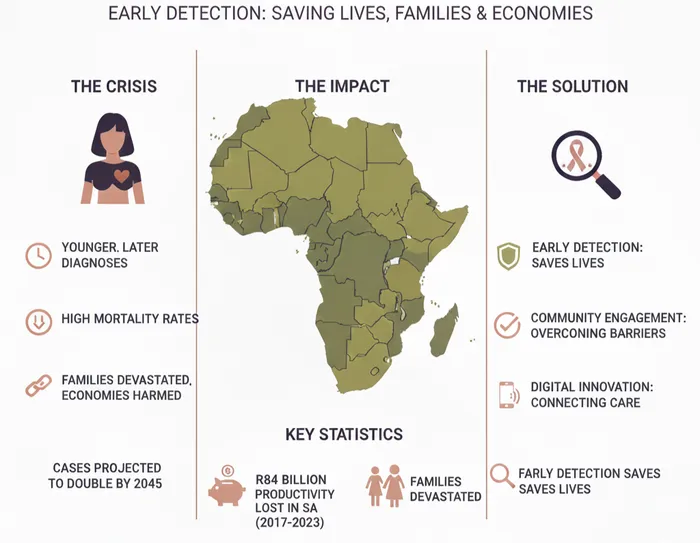
Image: Infographic
Digital innovation and community engagement
Digital tools are reshaping breast cancer care in low-resource settings. Mobile health applications, telemedicine, and secure digital platforms connect patients and specialists, overcoming distance and fragmentation.
“In low-resource environments, digital health does not need to be complicated to be transformative,” Benn told IOL.
“When clinicians across the country can review cases together, no woman is denied expert decision-making because of where she lives.”
Central is community engagement. Studies in South Africa have shown that social and cultural stigma, as well as traditional beliefs, often delay care.
And if there is one investment that will change outcomes, it is early detection and timely diagnosis,” Benn said.
A devastating consequence of late diagnosis is the rise of maternal orphans — children who have lost their mothers to breast cancer. Each mother we lose affects not just a family but a generation,” she added.
“Preventing a child from becoming a maternal orphan is one of the most powerful forms of social protection. Investing in women’s health is investing in children’s futures and community resilience.”
Early detection and timely treatment stabilise families and prevent long-term social and economic harm.
Priorities and Funding Recommendations
The Africa Breast Cancer Council is focused on practical, high-impact policies to meet the WHO's 2040 breast cancer goals: doubling early-stage diagnoses, reducing delays from symptoms to treatment, and improving survival figures from 50% to 80%.
“Our council is intentionally diverse - oncologists, surgeons, patient advocates, first ladies, academics, and former ministers - because changing outcomes requires influence at every level,” Benn explained.
Strengthening frontline systems whilst training primary healthcare workers, expanding community engagement, improving referral pathways, and ensuring access to quality imaging and pathology can shift breast cancer from a crisis defined by late presentation to a success story defined by survival.
A much needed service is training primary healthcare workers and engaging communities, which ensures timely attention, particularly in rural and underserved areas.
Vision of Hope
“I see the strength of African women and the determination of our clinicians every day,” she said. For Professor Carol Benn, her vision is a continent where every woman is heard early, diagnosed quickly, treated appropriately, and supported throughout her journey.
"With coordinated effort, we can build a future where early detection is the norm, survival is expected, and every woman feels supported, respected, and seen.”
As Chair of the Africa Breast Cancer Council, Benn calls on governments and international partners to focus on early detection in their funding strategies. Her closing remarks:
"If we can meet our objectives for timely diagnosis, we can significantly improve breast cancer outcomes across the continent."
IOL